What are the other Names for this Condition? (Also known as/Synonyms)
- Chemotherapy-Induced Pulmonary Fibrosis
- Cryptogenic Fibrosing Alveolitis
- Drug-Induced Pulmonary Fibrosis
What is Pulmonary Fibrosis? (Definition/Background Information)
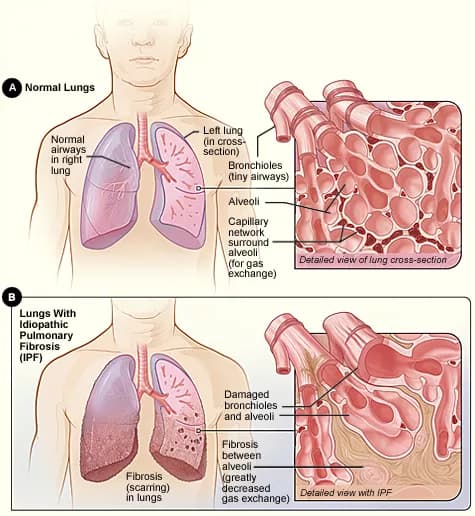
- Pulmonary Fibrosis refers to a condition when the lung tissues undergo inflammation and heal by scarring of the tissues. This formation of scar tissue is called fibrosis
- The scarring of the lungs makes it hard for them to function normally, resulting in certain typical symptoms such as breathing problems that not only affects the lungs, but also the entire body, as oxygen cannot be delivered efficiently to the body
- Pulmonary Fibrosis is diagnosed using several techniques such as through blood tests, chest x-ray, computerized axial tomography (CAT) scan, lung biopsy, bronchoscopy, and other diagnostic tools
- The most common form of Pulmonary Fibrosis is Idiopathic Pulmonary Fibrosis (IPF). Certain types of Pulmonary Fibrosis may be treated, if the causative agent is known
- A fibrotic lung, as a result of IPF, is usually not reversible. However, some medications may help in slowing disease progression and improving the quality of life
There are many types of Pulmonary Fibrosis and these include:
Idiopathic Pulmonary Fibrosis (IPF), also known as Cryptogenic Pulmonary Fibrosis/Alveolitis: This kind of Pulmonary Fibrosis is the most common type. As the name (idiopathic) suggests, the origin of IPF is unclear. However, it is thought to result from an inflammatory response following injury to the lungs leading to inflammation, which is followed by abnormal healing of the lungs by scarring.
There is an association of IPF with:
- Smoking
- Gastroesophageal reflux disease (GERD)
Drug-Induced Pulmonary Fibrosis: A number of commonly used drugs could potentially cause this type of fibrosis. These drugs and medications include:
- Medications that are used for treating heart ailments (amiodarone)
- Chemotherapy drugs
- Antibiotics that are used to treat some infections such as nitrofurantoin
- Seizure medications such as phenytoin
- High concentration of oxygen
Radiation-Induced Pulmonary Fibrosis: This condition is relatively common and follows radiation therapy administered to the chest region for certain cancers, such as breast, lung, and neck cancers.
Pulmonary Fibrosis Secondary to Connective Tissue Diseases:
- Systemic lupus is a chronic autoimmune disease causing inflammation and antibody production that attack several organs. Many lung abnormalities, including fibrosis, are observed in chronic lupus patients
- Rheumatoid arthritis (RA) is also an autoimmune disorder. Interstitial lung disease is the most common and most serious lung disorder associated with RA, and it generally leads to fibrosis. Certain medications used to treat RA could also lead to fibrosis of the lungs
- Systemic scleroderma is an autoimmune disorder as well, in which scar tissue is formed on the skin, and in many cases, in the internal organs
- Mixed connective tissue disease can also be associated with skin, joint, and lung problems
Sarcoidosis-Induced Fibrosis of the Lungs: Sarcoidosis is a disease that causes inflammation in the body tissues. Small lumps (granulomas or nodules) form as a result of the disease, and in more than 90% of the cases, the lungs get affected. When many small lumps form together in the lungs, it leads to scarring of the tissue.
Who gets Pulmonary Fibrosis? (Age and Sex Distribution)
- Pulmonary Fibrosis affects individuals between the ages of 40-70 years
- It is prevalent across all racial and ethnic groups
- A higher incidence of IPF is reported in men than women
What are the Risk Factors for Pulmonary Fibrosis? (Predisposing Factors)
The leading factors, known to be risk factors for Pulmonary Fibrosis are:
- Age: Pulmonary Fibrosis is more common in older adults
- Smoking
- Occupations, such as welding, mining, or farming, or involving asbestos exposure
- Cancer treatments such as chemotherapy and radiation (to the chest area)
- Health issues such as connective tissue disease, and the use of certain medications
- Hobbies such as bird keeping
- Genetic factors; as Pulmonary Fibrosis is known to run in some families
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Pulmonary Fibrosis? (Etiology)
The following are some of the known or suspected causes of Pulmonary Fibrosis:
- Exposure to asbestos, silica dust, grain dust, and other dust particles
- Smoking
- Use of some medications such as chemotherapy drugs, medicines used to control irregular heartbeats (like amiodarone), antibiotics (like nitrofurantoin), and rheumatologic medications (such as methotrexate)
- Radiation therapy
- Pre-existing medical conditions such as systemic lupus, rheumatoid arthritis, scleroderma, sarcoidosis, and many others
What are the Signs and Symptoms of Pulmonary Fibrosis?
Individuals with Pulmonary Fibrosis may present with one or more of the following signs and symptoms:
- Chest pain
- Cough
- Shortness of breath on exertion or dyspnea
- Loss of activity owing to muscle aches and fatigue
- Very low levels of oxygen in blood, also known as hypoxemia
- Blue-tinged skin or cyanosis, which is more clearly visible along the mouth or nails
- Clubbing, which is irregular enlargement around the nail bases in the fingers and toes
- Weight loss
How is Pulmonary Fibrosis Diagnosed?
A physician may employ several methods to diagnose Pulmonary Fibrosis. These include:
- Checking complete medical history including occupation, medication, hobbies, and bird exposure history, followed by a physical examination
- Test to measure oxygen levels
- Chest x-ray
- Pulmonary function test
- Computerized axial tomography scan (CAT scan) of the chest: It is common to have a high resolution CT scan of the lungs
- If necessary, a lung biopsy and/or a bronchoscopy may be performed
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Pulmonary Fibrosis?
Pulmonary Fibrosis could potentially lead to:
- An abnormally high number of red blood cells (RBCs) owing to low levels of oxygen
- Increased blood pressure in the lungs, also known as pulmonary hypertension
- A collapsed lung, leading to respiratory failure
- Lung cancer, especially when there is a history of smoking and asbestos exposure
- In some cases a heart failure (on the right side) because of an overworked right ventricle. This condition is termed as cor pulmonale
How is Pulmonary Fibrosis Treated?
A physician or a lung health professional, after thorough testing and diagnosis, may recommend one or more of the following treatment measures to help alleviate some of the symptoms of Pulmonary Fibrosis in the short term.
- The Food and Drug Administration (FDA) has approved two drugs for IPF (on October 15, 2014) - Pirfenidone (Esbriet) and Nintedanib (Ofev). These drugs have been found to slow the worsening of the disease
- Use of medications such as corticosteroids, sometimes combined with immunosuppressant drugs to reduce inflammation, especially in those with a history of connective tissue diseases
- It is not clear if acetylcysteine is beneficial for patients with IPF; trials are ongoing
- Commonly, steroids and steroid sparing medications, such as methotrexate and azathioprine, are prescribed for sarcoidosis-associated lung problems
- Oxygen therapy for patients with low blood oxygen levels
- Treatment for GERD with stomach acid suppressing medicines is important in patients with Pulmonary Fibrosis, particularly with IPF
- It is also recommended to sleep with 2 or 3 pillows in order to keep (prop) the head up, so as to prevent aspiration into the lungs
- Pulmonary rehabilitation: Patients may be referred to pulmonary rehabilitation centers to help them with:
- Breathing techniques and exercises
- Diet changes
- Exercise changes
- In the case that any/all of the above measures have been tried, but the disease gets severe or worse; then, lung transplantation may be an option
A qualified physician/specialist must be consulted for the treatment of Pulmonary Fibrosis. Patients with this condition require close supervision between primary care physicians and pulmonologists.
How can Pulmonary Fibrosis be Prevented?
A few preventive measures of Pulmonary Fibrosis may include:
- For Idiopathic Pulmonary Fibrosis, currently there are no known prevention techniques since the causative agent is unknown
- Avoiding smoking
- Reducing exposure to known causative agents such as asbestos, grain/wood/metal dust, and silica dust
- Wearing appropriate respirators and masks while performing jobs that involve dust, chemicals, and metals
What is the Prognosis of Pulmonary Fibrosis? (Outcomes/Resolutions)
- The prognosis is variable and is dependent on the cause of Pulmonary Fibrosis
- It is very important to avoid getting further exposure to the ‘reason’ for Pulmonary Fibrosis such as chemicals, dusts, metals, and medications. Any associated health conditions, such as connective tissue disease or sarcoidosis, needs to be treated
- Improvement in the patient’s quality of life and preventing decline in lung function may be achieved through a combination of medications, oxygen therapy at home, and through lifestyle changes
- IPF is generally not reversible; hence, attention should be paid if it is beneficial to start medications and acid reflux therapy
Additional and Relevant Useful Information for Pulmonary Fibrosis:
The following DoveMed website link is a useful resource for additional information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.