What are the other Names for this Condition? (Also known as/Synonyms)
- Cutaneous Melanoma In Situ
What is Melanoma In Situ of Skin? (Definition/Background Information)
- A melanoma is a type of cancer that develops from cells, called melanocytes. Melanocytes are cells that produce melanin - the pigment that gives skin its color
- A normal skin is composed of three layers:
- Epidermis - the outermost protective layer
- Dermis - the middle layer containing blood vessels, sweat glands, hair follicles, and nerves
- Subcutis - composed of fat, collagen strands, and vessels
The epidermis and dermis are separated by a layer, called the basement membrane.
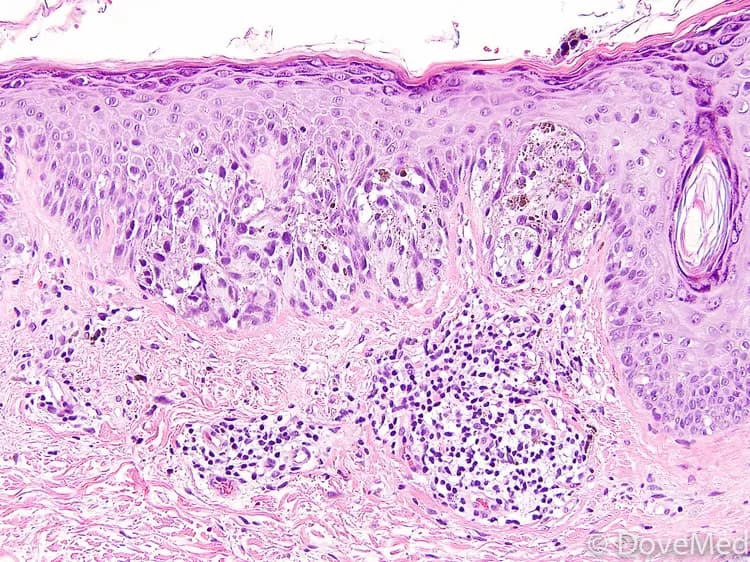
- Melanomas that are confined to the epidermis and have not yet penetrated through the basement membrane are called Melanoma In Situ of Skin. They are usually brown or black in color, but sometimes may be pink, tan, or white
- The term “in situ” means at the site of origin. Benign melanocytes are located at the base of the epidermis, just above the basement membrane. When melanocytes become malignant, if they remain at their original biological ‘habitat’, they are termed in situ
- Although melanomas may occur anywhere on the body, Cutaneous Melanoma In Situ or Melanoma In Situ of Skin generally occur on sun-exposed areas. Some of the common sites include:
- Chest and back in men
- Legs in women
- Neck and face
- Melanoma In Situ of Skin is diagnosed with the help of a biopsy. Once a definitive diagnosis is made, it is surgically removed (excised). The outcome for such cancer types, which have been diagnosed early and excised completely, is generally excellent
Who gets Melanoma In Situ of Skin? (Age and Sex Distribution)
- Melanoma In Situ of Skin can occur in young as well as old individuals. It is one of the most common cancers in people younger than 30 years
- In the United States, it has been observed that women are at an increased risk before the age of 40 years, while men are at a higher risk after the age of 40 years
- Cutaneous melanoma also occurs more frequently in Caucasians, as compared to individuals of other races
What are the Risk Factors for Melanoma In Situ of Skin? (Predisposing Factors)
The following factors increase the risk for Melanoma In Situ of Skin:
- Exposure to ultraviolet (UV) rays is a major risk factor. UV rays are present in sunlight, and also in tanning lamps and beds
- Nevus (medical term for mole) is a non-cancerous pigmented tumor. While most nevi never become cancerous (or malignant), a small number of atypical/dysplastic nevi (moles with abnormal shape/borders/color) may turn cancerous. When such dysplastic nevi run in families, the condition is called dysplastic nevus syndrome. Individuals with this condition have a 10% increased risk of developing melanoma. Despite the above and irrespective of the condition, whether the nevi are present since birth, or are normal, or atypical; the more the number of moles, the greater is the risk
- Fair-skinned individuals are at a higher risk; more so those with freckles or those who develop sun burns easily
- Previous history of melanoma or a history of melanoma in parents/siblings
- An inherited condition called xeroderma pigmentosum, where the ability of the cells to repair sun-induced damage to genetic material is impaired
- Weakened immune system, as a result of infections (such as HIV infection), medications (chemotherapy or immunosuppressants), or due to the presence of cancers (such as lymphoma)
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Melanoma In Situ of Skin? (Etiology)
The exact reason behind, why some moles turn cancerous and others do not, is still not exactly known. However, the potential causes for Melanoma In Situ Skin include:
- Uncontrolled activity of oncogenes (rogue genes that promote cell growth and division) or depressed action of tumor suppressor genes (genes that normally keep a check on cell growth and division) is thought to play a role in the development of melanomas
- About 50% of all melanomas have a mutation (change) involving the BRAF oncogene
- UV radiation induces damage to DNA (genetic material that determines all of our traits and functions), which in turn may turn on the oncogenes, or turn-off tumor suppressor genes
- In families with inherited melanomas, gene mutations that increase the risk for cancer are passed on from one generation to the next
What are the Signs and Symptoms of Melanoma In Situ of Skin?
Melanoma In Situ of Skin can develop from an existing mole or appear as a new spot. The signs and symptoms may include:
- A pigmented area that is Asymmetrical in shape, whose Borders are irregular or ragged
- A pigmented area that is not Colored uniformly, unlike a benign mole, which has an even distribution of shades
- Any suspicious looking spot, whose Diameter is more than ¼ inches (6 millimeters)
- Any suspicious looking spot that is Evolving, or changing in shape/color
These signs are often collectively referred to as the ‘ABCDE characteristics’ of melanoma by physicians. (Source: The Skin Cancer Foundation, New York)
- A suspicious looking spot or a ‘potential melanoma’ often differs in appearance from other benign moles on the body. This variability is sometimes called the ugly duckling sign by physicians (Source: The Skin Cancer Foundation, New York)
- A suspicious pigmented area/spot showing a spread of color to the surrounding skin and with any swelling, redness or itching (due to inflammation). Such areas may also be scaly, exhibit some oozing of fluid, or bleed
How is Melanoma In Situ of Skin Diagnosed?
A thorough history and a complete physical exam by a physician are crucial for the diagnosis of Melanoma In Situ of Skin. This is followed by some tests which include:
- Biopsy of skin: A sample of the skin from any suspected area found on physical examination, is taken and examined under a microscope for signs of cancer by a pathologist. The types of biopsy performed include:
- Excisional biopsy: After numbing the area with a local anesthetic, the entire mole is removed with a small border of surrounding skin. Where possible, this is the generally preferred method
- Punch biopsy: After numbing the area with a local anesthetic, a circular blade is pressed into the skin around the suspicious area and a round piece of skin removed. This type of biopsy is carried out when the lesion (the suspicious area) is large in size
- Incisional biopsy: After numbing the area with a local anesthetic, a portion of the tumor is removed using a surgical knife
- Shave (tangential) biopsy: In situations where the thinness of the lesion can be determined clinically, a sharp blade-scalpel or flexible razor blade is used to remove a representative portion of the pigmented lesion
- Some physicians perform additional screening, such as chest X-ray or blood test, to check for any possible spread
According to the American Joint Committee on Cancer TNM system, Melanoma In Situ is categorized as stage-0 (Tis, N0, M0) meaning that the tumor is confined to the epidermis and there is no involvement of the lymph nodes or other distant organs.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Melanoma In Situ of Skin?
By definition, Melanoma In Situ of Skin should have no risk of metastatic disease. This is because the malignant cells can only spread to other tissues via blood vessels or lymphatic vessels. These pathways are below the basement membrane, so they are not available to the cells of Melanoma in Situ of Skin. The absence of risk of spread is dependent upon microscopic examination of a specimen diagnosed as being “in situ” with great reliability.
How is Melanoma In Situ of Skin Treated?
Melanoma In Situ of Skin may be treated as follows:
- When a diagnosis of Melanoma In Situ is made after a biopsy, a re-excision of the original site is done along with some surrounding area of normal, non-cancerous skin (called a margin)
- The extent of the margin is determined by a surgeon after considering a number of factors while although commonly, a margin of 0.5 centimeters in every direction around the original cancer is accepted as standard
- This excision is done under a local anesthetic in most cases
- For cosmetic reasons, a skin grafting (placing normal skin over the wound area) may be performed
- Mohs assisted excision will often be used for large lesions in locations with high risk of negative functional and cosmetic outcomes
How can Melanoma In Situ of Skin be Prevented?
A few steps to prevent of Melanoma In Situ of Skin include:
- Avoid direct exposure to UV rays and remain in the shade, as and when possible
- When heading out in sun:
- Slip on a shirt
- Slop on some sunscreen. Sunscreens with SPF values higher than 30, and those offering broad spectrum protections (against UV-A and UV-B rays) are recommended. Apply an ounce to all exposed areas 30 minutes before heading outdoors. Reapply every two hours, and also after excessive sweating
- Slap on a hat
- Wrap on sunglasses
This is encapsulated as the “Slip! Slop! Slap! Wrap” method for skin cancer prevention. (Source: The American Cancer Society, Atlanta)
- Avoid tanning beds and sun lamps
- Perform self-examination of skin from head to toe, once a month
- Get a professional skin exam from a healthcare provider, once a year
- All patients with melanoma should undergo skin examinations regularly even after treatment, at least once a year throughout their lives
What is the Prognosis of Melanoma In Situ of Skin? (Outcomes/Resolutions)
A majority of individuals with Melanoma In Situ of Skin have an excellent prognosis following complete excision of the tumor.
- Almost all those who are diagnosed with stage-0 disease, survive for 5-10 years after diagnosis. The overall 5- or 10-year survival rates are 99-100%
- If Melanoma in Situ of Skin recurs at the surgical margin of the prior excision, prognosis is still excellent if the lesion is still entirely Melanoma in Situ when the re-excision is examined microscopically
Additional and Relevant Useful Information for Melanoma In Situ of Skin:
- Melanoma is the most common form of cancer in young adults aged 25-29 years. About 1 in 50 Americans have a lifetime risk of developing melanoma
- The ‘Slip-Slop-Slap campaign’ was initially launched in Australia, by Cancer Council Victoria in the 1980s, to promote awareness about skin cancer and methods for its prevention. This was then adopted in New Zealand as the ‘Slip-Slop-Slap-Wrap campaign’ (Source: The Wikipedia)
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.