What are the other Names for this Condition? (Also known as/Synonyms)
- EIC (Epidermal Inclusion Cyst)
- Inclusion Cyst
- Keratin Cyst
Sebaceous cyst - this is a commonly used name for EIC, although it misidentifies the origin and contents of Epidermal Inclusion Cyst.
What is Epidermal Inclusion Cyst? (Definition/Background Information)
- Epidermal Inclusion Cyst (EIC) is a very common and benign skin cyst that is usually seen in young and middle-aged adults
- The risk factors for Epidermal Inclusion Cysts may include the presence of acne, long-term sun exposure, and repeat trauma to the skin. However, many of them are known to occur in a sporadic manner
- The cysts may occur anywhere in the body; the common sites are the face and trunk region. In most cases, Epidermal Inclusion Cysts do not present any pain or other significant signs and symptoms. When EICs grow, the process is usually very slow
- Typically, for asymptomatic and non-infected cysts, no treatment may be necessary, as Epidermal Inclusion Cysts are known to resolve by their own
- Large and infected cysts may be surgically excised/removed. The prognosis of Epidermal Inclusion Cyst is excellent with suitable treatment, although the cysts are known to recur
Who gets Epidermal Inclusion Cyst? (Age and Sex Distribution)
- Epidermal Inclusion Cyst (EIC) can affect individuals of any age, although they are commonly observed in young and middle-aged adults in the 20-40 years’ age category
- Both males and females may be affected. Men are affected more than women in a 2:1 ratio
- Individuals of all racial and ethnic background may be affected. Worldwide, no geographical localization of EIC has been reported
What are the Risk Factors for Epidermal Inclusion Cyst? (Predisposing Factors)
The risk factors for Epidermal Inclusion Cyst (EIC) include the following:
- Individuals with acne vulgaris have a higher risk for EIC
- Skin damage from chronic or long-term sun exposure, often for several decades; this is particularly noted in older adults
- In rare cases, EICs are associated with certain genetic disorders including:
- Gardner syndrome
- Favre-Racouchot syndrome
- Gorlin syndrome (basal cell nevus syndrome)
- Use of medications, such as BRAF inhibitors (imiquimod and cyclosporine), are known to increase the risk for EIC on facial skin
- Repeat trauma of the hair follicles
- Human papillomavirus (HPV) infection
- In a majority of cases, no risk factors are clearly identified, and the cysts are known to form sporadically
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Epidermal Inclusion Cyst? (Etiology)
The cause of development of Epidermal Inclusion Cyst (EIC) is unknown in a majority of cases since many of them occur sporadically. The cysts are known to form when the tiny hair follicle orifices get plugged from factors such as preexisting acne or minor trauma.
Epidermal Inclusion Cysts are classified as primary and secondary.
- In primary EIC, the cysts form directly from the hair follicle infundibulum (the funnel-shaped upper segment of the hair shaft), when the hair follicle becomes obstructed
- Secondary EIC is observed against a background of trauma, acne, or other factors
Other contributory factors include prolonged sun exposure, use of certain medications, and infections from human papillomavirus. Very rarely, EICs are observed to form in a setting of certain genetic syndromes such as Gardner syndrome.
Epidermal Inclusion Cysts are not contagious, and they do not spread from one individual to another via direct or indirect physical contact.
What are the Signs and Symptoms of Epidermal Inclusion Cyst?
Epidermal Inclusion Cysts are generally asymptomatic. In some, the signs and symptoms observed may include:
- The cysts appear as tiny nodules just below the skin surface with a visible central punctum
- The cysts can range in size from a few mm to several cm; small cysts may not be even noticeable
- These cysts are usually painless and non-itchy
- They are mostly well-demarcated and firm to touch
- If the lesions are infected, then they may rapidly increase in size, appear reddish in color, and can become painful
- Large cysts are generally known to rupture
- Epidermal Inclusion Cysts can occur at any location on the body
- They are generally seen at skin sites of trauma, inflammation, or within the vicinity of acne lesions
- The most common sites include the face, including the scalp and neck region, the trunk, and scrotum
- The lesions may grow/enlarge or remain stable in size
In the setting of a genetic disorder, numerous cysts may be present and/or the cysts may be found at several locations on the body.
How is Epidermal Inclusion Cyst Diagnosed?
A diagnosis of Epidermal Inclusion Cyst may involve the following:
- Complete physical examination and a thorough medical history
- Dermoscopy: It is a diagnostic tool where a dermatologist examines the skin using a special magnified lens
- Wood’s lamp examination: In this procedure, the healthcare provider examines the skin using ultraviolet light. It is performed to examine the change in skin pigmentation
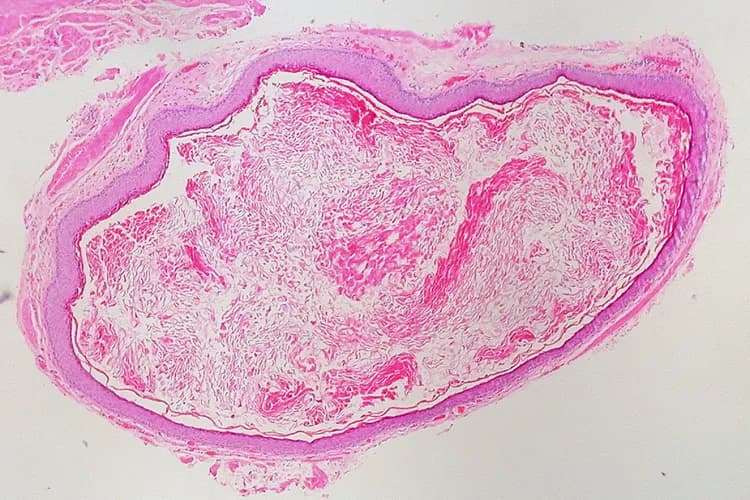
- Skin biopsy: A skin biopsy is performed and sent to a laboratory for a pathological examination. The pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis. A skin biopsy may not be generally necessary to diagnose the condition
- Specific tests may be undertaken based on the presence of any underlying disorder
A differential diagnosis may be undertaken to exclude the following conditions prior to definitively diagnosing EIC:
- Abscess on the skin
- Benign skin growths
- Brachial cleft cyst
- Calcinosis cutis
- Dermoid cyst
- Ganglion cyst
- Lipoma
- Neurofibroma
- Neuroma
- Pachyonychia congenita
- Pilar cyst
- Pilomatrixoma
- Pilonidal cyst
- Skin cancers and metastatic skin lesions
- Steatocystoma simplex and steatocystoma multiplex
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Epidermal Inclusion Cyst?
Epidermal Inclusion Cysts (EICs) are benign cysts that generally do not cause any significant complications. However, the following factors may be a cause of concern:
- The presence of large-sized cysts may result in cosmetic issues
- Superimposed bacterial or fungal infection may develop at the lesion site
- Localized cellulitis
- Sometimes, they can become infected, rupture, and release pus. This condition is called a ruptured Epidermal Inclusion Cyst. When these heal, they can leave a scar behind
- Infected Epidermal Inclusion Cysts typically will not grow a pathogenic (disease-causing) bacterium on culture
- Most of the redness, swelling, and pain are caused by the non-infectious contents stimulating an inflammatory response similar to an actual infection
- Recurrence of the condition after treatment, especially from incomplete excision of the cyst
- In rare cases (less than 1% of the cases), a basal cell carcinoma or squamous cell carcinoma is known to arise from the EIC following a malignant transformation
- Complications may arise from the underlying skin disorder
How is Epidermal Inclusion Cyst Treated?
The treatment of Epidermal Inclusion Cyst (EIC) may involve the following:
- In a majority of cases, removal of the cyst is not necessary, unless the cyst causes bothersome signs and symptoms and cosmetic issues
- Intralesional injections may be considered for inflamed cysts based on the healthcare expert’s evaluation. This can help prevent infection and avoid surgical incision and drainage of the cyst
- A definitive treatment for EIC is its complete surgical excision, which can result in a cure and prevent recurrences
- Surgical removal of large infected or inflamed EIC can be more complex or large than warranted. In that setting, these lesions can be incised and drained
- A small opening is cut into the center of the cyst, and the contents removed by pressure, or the use of an instrument placed through the incision
- In large lesions in which complete drainage is not certain, a sterile gauze wick is inserted to permit further drainage. A short section of wick is left outside, to permit its removal at a subsequent visit
- Treating any superimposed infections suitably (antibiotic therapy for bacterial infections)
- Treating the underlying health condition, if any present, is also important
Sometimes, treatment may not be necessary even for large and inflamed cysts that are not infected. These are known to resolve spontaneously.
How can Epidermal Inclusion Cyst be Prevented?
Currently, there are no known methods available to prevent the occurrence of Epidermal Inclusion Cysts.
- However, prompt treatment of any skin conditions, such as acne or skin trauma, may help lower one’s risk
- Avoiding direct sun exposure through sun protection creams and wide-brimmed hats is beneficial
- Medications that are known to cause the condition may be discontinued
What is the Prognosis of Epidermal Inclusion Cyst? (Outcomes/Resolutions)
- The prognosis for Epidermal Inclusion Cyst is generally excellent with appropriate treatment since it is a benign cyst
- However, even with surgery, recurrences have been observed. The recurrence rate reported is between 1% to 8%
Additional and Relevant Useful Information for Epidermal Inclusion Cyst:
- There is no evidence to prove that oily foods and chocolate-based products have an influence on the development of Epidermal Inclusion Cyst
- Cleaning the skin too hard with strong chemicals or soaps may aggravate the skin condition. Care must be taken avoid strong soaps and chemicals that could potentially worsen the condition
The presence of dirt on the body is not a causative factor for the condition. However, it helps to be clean and hygienic, which may help the condition from getting worse
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.