What are the other Names for this Condition? (Also known as/Synonyms)
- Cutaneous Desmoplastic Melanoma
- DM of Skin
- Malignant Melanoma of Skin, Desmoplastic Type
What is Desmoplastic Melanoma of Skin? (Definition/Background Information)
- A melanoma is a type of cancer that develops from cells, called melanocytes. Melanocytes are cells that produce melanin; the pigment that gives skin its color
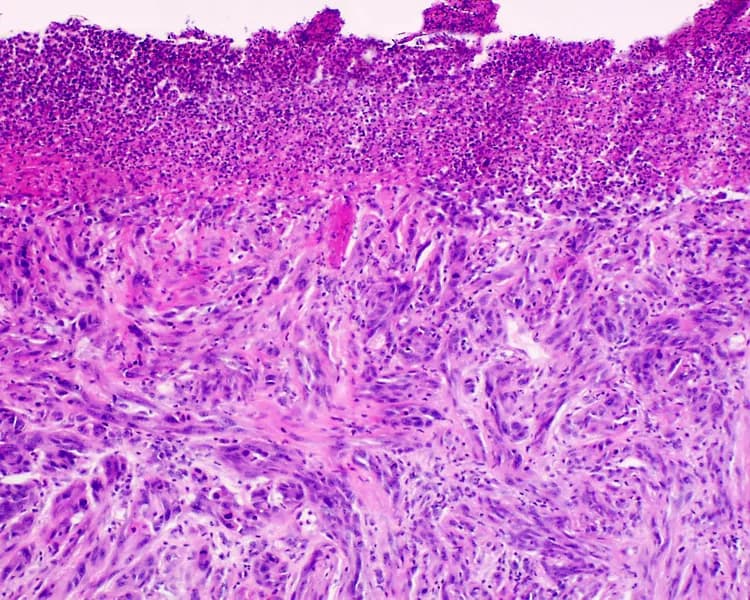
- Desmoplastic Melanoma (DM) of Skin is an uncommon subtype of cutaneous melanoma that usually arises from sun-exposed skin sites. It is seen in young and old adults
- In around 30% of the cases, the tumor is associated with neurotropism (a tendency to involve or proliferate along the path of the nerve cells and its surrounding tissues); in such cases, it is known as Desmoplastic Neurotropic Melanoma
- Desmoplastic Melanoma of Skin may initially start as a painless nodule or plaque; many tumors may lack pigmentation. The most common site is the head and neck region. Advanced tumors can invade deep into the subcutaneous tissues and even involve the bones
- Desmoplastic Melanoma of Skin is diagnosed with a confirmatory biopsy. The tumor can pose diagnostic challenges to a pathologist, since it can resemble a scar tissue. Once a definitive diagnosis has been made, it is surgically removed (excised). Some tumors are known to respond to radiation therapy
- The outcome of Desmoplastic Melanoma of Skin is generally guarded due to the aggressive nature of the tumor. Following its surgical removal, a high rate of tumor recurrence is observed
Who gets Desmoplastic Melanoma of Skin? (Age and Sex Distribution)
- Desmoplastic Melanoma of Skin is generally seen in the age range of 25-90 years, with a median age of 62 years
- Both males and females are seen with this condition, though a male predominance is indicated (7:4 male-female ratio according to some studies). But, desmoplastic melanomas seen on the arms/legs are mostly found in females
- Cutaneous melanomas occur more frequent in Caucasians, as compared to other races
- Between 1-4% of all diagnosed melanomas are of the desmoplastic type
What are the Risk Factors for Desmoplastic Melanoma of Skin? (Predisposing Factors)
The following factors may increase the risk for Desmoplastic Melanoma of Skin:
- Severe exposure to ultra violet (UV) rays is a major risk factor, especially during one’s childhood (and to some extent during one’s adulthood). UV rays are present in sunlight and also in tanning lamps and beds
- Radiation therapy undertaken for other medical conditions/cancers; the irradiated skin surface may be more prone to desmoplastic melanoma development
- A nevus (medical term for mole) is a non-cancerous pigmented tumor. While most nevi never become cancerous (or malignant), a small number of atypical/dysplastic nevi (moles with abnormal shape/borders/color) may turn cancerous. When such dysplastic nevi run in families, the condition is called dysplastic nevus syndrome. Individuals with this condition have a 10% increased risk of developing melanoma. Despite the above and irrespective of the condition, whether the nevi are present since birth, or are normal, or atypical; more the number of moles, more is the risk for melanoma
- Fair-skinned individuals are at a higher risk; more so those with freckles or those who develop sunburns easily
- Individuals with light or red hair color and those with blue eyes also have a higher risk
- Previous history of melanoma or a history of melanoma in parents/siblings; 6-14% of the individuals with melanoma are found to have someone with melanoma in their family
- An inherited condition called xeroderma pigmentosum, where the ability of the cells to repair sun-induced damage to genetic material is impaired
- Weakened immune system, as a result of infections (such as caused by the HIV), drugs (chemotherapy or immunosuppressants), and the presence of cancers (such as lymphoma)
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one's chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Desmoplastic Melanoma of Skin? (Etiology)
The potential causes of Desmoplastic Melanoma of Skin may include:
- Uncontrolled activity of oncogenes (rogue genes that promote cell growth and division) or depressed action of tumor suppressor genes (genes that normally keep a check on cell growth and division) is thought to play a role in the development of melanomas
- UV-radiation induces damage to DNA (genetic material that determines all of our traits and functions), which in turn may turn-on oncogenes, or turn-off tumor suppressor genes
- Both melanomas, inherited or acquired/sporadic, show genetic mutations and chromosomal anomalies, which are being currently characterized or researched upon
- About 50% of all melanomas have a mutation (change) involving the BRAF oncogene; however, BRAF gene mutations are only rarely observed in Cutaneous Desmoplastic Melanoma
- In families with inherited melanomas, gene mutations that increase the risk of cancer are passed on from one generation to the next
- Some cases of desmoplastic melanoma have been observed as metastasis from other melanoma forms; some are also seen to occur as recurrences
What are the Signs and Symptoms of Desmoplastic Melanoma of Skin?
Desmoplastic Melanoma of Skin may occur in a previously benign mole in some cases; de novo melanomas may be seen in other cases. The signs and symptoms may include:
- All the signs of a cutaneous melanoma, including a rapidly-growing, irregular-shaped pigmented area on the skin that is changing, can be seen. The ABCDE features may be noted
- In the case of desmoplastic melanoma, nearly 50% of the lesions do not show any remarkable pigmentation. They may be dull-colored or pale and resemble other skin tumors, such as a dermatofibroma, a scar, or another type of skin cancer called basal cell carcinoma
- Pigmented lesions are often found due to the presence of other melanoma types (including superficial spreading and lentigo maligna melanomas)
- The sun-exposed skin areas are commonly affected with the head and neck area (nose, ears, and lips) being the most common site, in about 37% of the cases
- Other sites include the limbs (mostly in women) and shoulders. Very infrequently, desmoplastic melanoma has been reported on the vulva too
- The skin may lose its elasticity and textural quality; hair loss may be observed in the affected skin area
- Sometimes, the presence of inflamed red nodules may be seen
- Bleeding lesions and ulcerations are uncommon
- Some skin lesions may not have any signs and symptoms during the initial stages
How is Desmoplastic Melanoma of Skin Diagnosed?
A thorough history and a complete physical exam by a physician are crucial for the diagnosis of Desmoplastic Melanoma of Skin. This is followed by some tests which include:
- Biopsy of skin: A sample of the skin, from any suspected area found on physical examination, is taken and examined under a microscope for signs of cancer by a pathologist. The types of biopsy performed include:
- Excisional biopsy: After numbing the area with a local anesthetic, the entire mole is removed with a small border of surrounding skin. Where possible, this is the generally preferred method
- Punch biopsy: After numbing the area with a local anesthetic, a circular blade is pressed into the skin around the suspicious area, and a round piece of skin removed. This type of biopsy is carried out, when the lesion (the suspicious area) is large in size
- Incisional biopsy: After numbing the area with a local anesthetic, a portion of the tumor is removed using a surgical knife. This provides more tissue for examination than a punch biopsy
- Sentinel lymph node biopsy: Performed to determine if the melanoma has spread to nearby lymph nodes. A dye is injected into the area from where the melanoma was removed. The first lymph node that takes up the dye is biopsied and examined for cancer cells, under a microscope
- Sometimes, biopsy of other large lymph nodes in the area near the melanoma may be performed using fine needle aspiration cytology (FNAC) technique. In this, a sample of cells is removed from the mass, using a syringe with a hollow needle and then examined under a microscope
- If the melanoma is suspected to have metastasized (spread) to internal organs, imaging tests, such as X-ray, CT scan or MRI of the affected areas, may be carried out
- In rare cases, biopsies of areas other than skin may have to be done, when the primary source/origin of the tumor cannot be determined
A differential diagnosis to exclude the following conditions should be undertaken:
- Dermatofibroma
- Desmoplastic and Spitz nevi
- Malignant tumors including malignant fibrous histiocytoma, fibrosarcoma, leiomyosarcoma, and malignant peripheral nerve sheath tumor
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Desmoplastic Melanoma of Skin?
The more advanced cases of Desmoplastic Melanoma of Skin metastasize beyond the skin, to the local and regional lymph nodes and other organs. Organs that are commonly involved in metastasis include the following:
- Lung
- Liver
- Brain
- Bone
- Gastrointestinal tract
Desmoplastic melanomas are known to infiltrate deep into the skin tissues and even affect the underlying bones and glands. Tumors on the head and neck region may affect the skull bones, the salivary glands, etc. Recurrences following incomplete surgical excision are commonly noted.
How is Desmoplastic Melanoma of Skin Treated?
The choice of treatment for Desmoplastic Melanoma of Skin depends on how far the cancer has progressed. This is estimated through staging of the tumor. Some of the factors taken into consideration during staging include:
- The thickness of the melanoma (also called Breslow’s measurement): Tumors can be thin, intermediate, or thick, depending on how deep into the skin they have penetrated. The thinner the tumor, the better the chances of a cure
- Presence of any ulceration (open sores) over the tumor
- Spread of melanoma to lymph nodes or other internal organs
The melanoma is sorted into one of four stages depending on how far it has progressed, with I and II being early stages, III and IV being later stages, where melanoma has spread to sites beyond the skin. While early stage melanomas can be treated by surgery alone, the later stages of the disease often require a combination of treatment measures. The advances in metastatic melanoma made in the last decade has led to improved survival rates for melanoma patients.
Treatment options for melanoma include:
Surgery:
- Simple excision of the tumor along with some normal, non-cancerous skin at the edges (called margin). The width of the margin is based on the thickness of the tumor; as the thickness of the melanoma increases, the margin required increases as well
- Mohs micrographic surgery:
- Being used of late by some surgeons as an alternative technique to standard excision of melanoma
- A thin layer of skin is removed and checked for cancer. This process is the carried out continuously, until a cancer-free specimen of skin is obtained, meaning the base of the defect is free of tumor
- This procedure is most often used as a surgical treatment option for thin early melanomas, and in cosmetically sensitive locations such as the face
- Lymph node dissection, in cases where the melanoma has spread to involve the nodes: Lymph nodes help in drainage of tissue fluid (lymph). However, removal of these nodes may therefore lead to a build-up of lymph causing swelling (lymphedema)
Chemotherapy:
- Drugs are used to kill the tumor cells, which may be given as oral pills, or injected into veins
- Side effects of chemotherapy may include nausea, vomiting, hair loss, loss of appetite, diarrhea, and fatigue, increased risk of infection, mouth sores, or easy bruising, depending on the drug used
- In cases, where the melanoma is advanced, but remains confined to an arm or leg; chemotherapy is only circulated through the affected the limb, by a process called isolated limb perfusion
Immunotherapy:
- This therapy stimulates the immune system and involves the use of substances produced naturally by the body or such similar synthetics, made in a laboratory
- Drugs used include, synthetic immune proteins and proteins that boost the immune system, called cytokines- interferon alpha or interleukin-2
- Side effects of cytokines may include chills, fatigue, fever, headaches and muscle aches; while synthetic immune proteins may cause the immune system to start attacking other parts of the body
Targeted therapy:
- Involves the use of drugs tailored to target the differences in a melanoma cell, as compared to a normal cell
- Half of all melanomas involve a mutation in the BRAF gene. This is targeted by a drug vemurafenib
- Side effects may include nausea, joint pain, fatigue, rash, itching, hair loss, sensitivity to the sun, and rarely heart rhythm problems, liver problems, severe allergic reactions, and severe skin or eye problems
Radiation therapy: This is observed to be effective in some cases.
- This uses high energy beams to kill cancer cells
- Generally, this method is not used to treat the original melanoma, but often to relieve symptoms, when the melanoma has spread to other organs; or following lymph node dissection, where many nodes were found to be cancerous
- The most common side effect is fatigue, but this gets resolved, once the treatment is complete
How can Desmoplastic Melanoma of Skin be Prevented?
A few steps to prevent of Desmoplastic Melanoma of Skin may include:
- Avoid direct exposure to UV rays and remain in the shade, as and when possible
- When heading out into the sun:
- Slip on a shirt
- Slop on some sunscreen. Sunscreens with SPF values higher than 30, and those offering broad spectrum protections (against UV-A and UV-B rays), are recommended. Apply an ounce to all exposed areas, 30 minutes before heading outdoors. Reapply every two hours, and also after excessive sweating
- Slap on a hat
- Wrap on sunglasses
This is encapsulated as the “Slip! Slop! Slap! Wrap” method for skin cancer prevention. (Source: The American Cancer Society, Atlanta)
- Avoid tanning beds and sun lamps
- Perform self-examination of your skin, from head to toe, once a month
- Get a professional skin exam from a healthcare provider, once a year
- All patients with melanoma should undergo skin examinations regularly even after treatment, at least once a year throughout their lives
What is the Prognosis of Desmoplastic Melanoma of Skin? (Outcomes/Resolutions)
- The prognosis of Desmoplastic Melanoma of Skin is similar to other forms of cutaneous melanoma. The overall 5 year survival rate is about 79%, and the 2 year recurrence rate is high at around 78%
- Individuals with early-stage melanoma have better outcomes compared to those with more advanced melanoma, where the cancer has spread to lymph nodes or other organs
- The following factors are known to affect the prognosis:
- High cell division rate
- Tumor thickness and ulceration
- Neurotropism
- Male gender
- Site of the tumor
In general, the prognosis depends upon a set of several factors, which include:
- Stage of tumor: With lower-stage tumors, when the melanoma is confined to site of origin, the prognosis is usually excellent with appropriate therapy. In higher-stage cancers, such as those with metastasis, the prognosis is poor
- Overall health of the individual: Individuals with overall excellent health have better prognosis compared with those with poor health
- Age of the individual: Older individuals generally have poorer prognosis than younger individuals
- The size of the melanoma: Individuals with small-sized melanomas fare better than those with large-sized ones
- Individuals with bulky disease have a poorer prognosis
- Involvement of vital organs may complicate the condition
- The surgical resectability of melanoma of skin (meaning, if the melanoma can be removed completely)
- Whether the cancer is occurring for the first time, or is recurrent. Recurring cancers have worse prognosis compared to those that do not recur
- Response to treatment: Melanomas that respond well to treatment have better prognosis compared to melanomas that do not respond to treatment
- Progression of the condition makes the outcome worse (progressive cutaneous melanoma)
Additional and Relevant Useful Information for Desmoplastic Melanoma of Skin:
- Melanoma is the most common form of cancer in young adults, aged 25-29 years. 1 in 50 Americans, have a lifetime risk of developing melanoma
- The ‘Slip-Slop-Slap campaign’ was initially launched in Australia, by Cancer Council Victoria in the 1980s, to promote awareness about skin cancer and methods for its prevention. This was then adopted in New Zealand as the ‘Slip-Slop-Slap-Wrap campaign’ (Source: The Wikipedia)
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.