Cardiomyopathy
What are the other Names for this Condition? (Also known as/Synonyms)
- CMP (Cardiomyopathy)
What is Cardiomyopathy? (Definition/Background Information)
- Cardiomyopathy (CMP) is a term used for the condition that affects the muscles of the heart. It can either be inherited (primary) or develop as a consequence of other diseases (secondary)
- Irrespective of how the disease develops, it leads to a weakening of heart muscles, such that the function of pumping blood to the rest of the body gets affected
- The disorder is classified into the following types:
- Hypertrophic Cardiomyopathy, in which there is a thickening of the walls dividing the four chambers of the heart and/or just the lower left chamber, known as the left ventricle. This subtype can further be classified on the basis of whether it is inherited (familial hypertrophic) or acquired; and, if it blocks the blood flow in the left ventricle (termed obstructive hypertrophic) or not (termed non-obstructive hypertrophic)
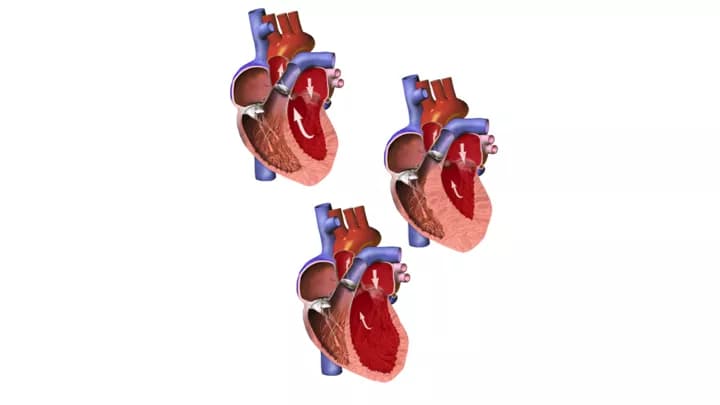
- Dilated Cardiomyopathy, a condition where the chambers of the heart are enlarged or weakened
- Restrictive Cardiomyopathy, which is a disorder of the contraction and relaxation of heart muscles
- Arrhythmogenic Right Ventricular Cardiomyopathy, which is characterized by the disintegration of the cardiac muscle
- Takotsubo Cardiomyopathy, which was first described in Japan, wherein an individual who experiences extreme emotional or physical stress has symptoms similar to a heart attack
- In general, the variety of risk factors for the different subtypes of CMP include a family history of the condition, certain chronic health conditions, infections, structural heart abnormalities, obesity, heavy smoking, alcoholism, neuromuscular disorders, exposure to toxins, immune deficiency diseases, such as HIV/AIDS infections, and cancers
- Cardiomyopathy may be inherited, can develop because of sporadic mutations, or develop secondary to an underlying medical condition.
- When inherited, mutations(s) in several genes are known to cause different subtypes of CMP. Some such genes, whose roles have been characterized, include MYH7, MYBPC3, TNNT2, TNNI3, DSP, JUP, PKP2, DSG2, DSC2, TNNI3 and TTN. These gene mutations can be inherited in an autosomal dominant, autosomal recessive, or X-linked manner. Some sporadic, non-heritable mutations are also known to cause Cardiomyopathy. However, the cause and nature of such mutations is not known
- The condition can also result from pre-existing medical ailments, such as diabetes, thyroid disease, congenital heart abnormalities, cancers, treatment for cancers, autoimmune disorders, neuromuscular disorders, connective tissue abnormalities, obesity, alcoholism, drug abuse, compromised immunity, and extreme physical or emotional stress
- Some individuals with Cardiomyopathy may be asymptomatic. In those with disease manifestation, symptoms can vary in severity, and may include breathlessness while exercising or resting, fainting after physical exertion, cough and shortness of breath while sleeping, chest pain, palpitations, swelling of ankles, legs and abdomen, tiredness, and lack of concentration, among others
- Some potential complications of the condition include backflow of blood into the heart (heart valve regurgitation), aberrant heart beats (arrhythmia), sudden cardiac arrest, development of blood clot, edema (fluid build-up), embolism, and stroke. Many of these complications can be fatal, if left untreated
- The diagnosis of the condition involves a thorough physical examination and an assessment of symptoms, family medical history evaluation, echocardiography (ECG), electrocardiography (EKG), stress test, chest X-ray and coronary catheterization. A biopsy of the heart muscle may be required for an accurate diagnosis, in some cases
- Cardiomyopathy is treated depending on the severity of symptoms. If the symptoms are mild, certain lifestyle changes, such as losing excess weight and reducing alcohol consumption, may be recommended. Medications to normalize heart rhythm, regulate blood pressure and remove toxins may be prescribed for this condition. Surgery to repair heart tissue or place a device, such as a defibrillator, may be required. A heart transplant may become necessary in individuals who have stopped responding to other treatments
- If Cardiomyopathy is caused by heritable genetic mutations, currently there are no guidelines available to prevent its occurrence. If the cardiac disease is secondary to an existing medical condition, then seeking medical attention for the underlying condition may help prevent its progression
- The prognosis of Cardiomyopathy is determined by the subtype, the individual’s general state of health and responsiveness to treatment. Some subtypes such as Takotsubo Cardiomyopathy report recovery within weeks of a cardiac episode. On the other hand, individuals with restrictive or dilated subtypes may succumb to the disease within 5-7 years of diagnosis
Who gets Cardiomyopathy? (Age and Sex Distribution)
- Cardiomyopathy is reported in individuals from around the globe, without any racial or gender predilection in its occurrence, except:
- Males are more prone to developing dilated (3:1 male-female ratio)) and arrhythmogenic Cardiomyopathy when compared to females
- Individuals of African descent develop dilated Cardiomyopathy more frequently than Caucasians
- Those with Greek or Italian ancestry have an increased possibility of being diagnosed with arrhythmogenic right ventricular Cardiomyopathy
- Restrictive Cardiomyopathy in children is more frequent in girls
- Takotsubo Cardiomyopathy affects predominantly post-menopausal women
- An accurate calculation of the occurrence rate of Cardiomyopathy may not be possible, as it may go undiagnosed in many instances. However, it is estimated that about 1 in every 500 adults may be having some form of Cardiomyopathy
- Typically, symptoms start appearing in adulthood in most cases. In children born with the congenital and restrictive subtypes of this disorder, disease manifestation occurs in the 5-6 year’ age group
What are the Risk Factors for Cardiomyopathy? (Predisposing Factors)
The following are some known risk factors for developing Cardiomyopathy:
- Having a family history of the condition
- Chronic high blood pressure
- Diabetes, particularly with poor glycemic control
- Diseases of the thyroid gland
- Excess growth hormone in the body (acromegaly), owing to a tumor in pituitary gland
- Hormonal imbalances due to tumor in adrenal glands (pheochromocytoma)
- Tumors of the brain and spinal cord (neurofibromatosis)
- Heart tumors
- A genetic disorder in body fat generation, storage and distribution, known as lipodystrophy
- Viral or bacterial infection in the heart muscle
- Connective tissue disorders
- Neuromuscular diseases, such as muscular dystrophy
- Hemochromatosis
- Sarcoidosis
- Amyloidosis
- Scleroderma
- Cancer treatments, such as chemotherapy
- Being on certain medications for psychiatric disorders
- Abuse of recreational drugs; alcoholism; heavy smoking
- HIV infection and AIDS
- Structural defects in the heart
- Heavy metal toxicity
- Obesity; sedentary lifestyle
- Advancing age
- Emotional stress that may be caused due to:
- Death in the family
- Illness
- Anxiety over a medical procedure, surgery, prognosis or test
- Emotional and/or physical abuse
- Loss of job or a financial setback
- Extreme fear
- Other phobias, such as glossophobia, or dread of addressing an audience
- Accident/injuries
- Having undergone a major surgery
- An attack of asthma
- Anxiety disorder
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Cardiomyopathy? (Etiology)
The cause of Cardiomyopathy may be genetic or sporadic. The following subtypes of CMP may be caused by heritable genetic changes:
Hypertrophic Cardiomyopathy is caused by mutations in MYH7, MYBPC3, TNNT2, TNNI3, and some unidentified genes.
- Under normal circumstances, these genes code for proteins involved in the formation of muscle structures called sarcomeres, which help the heart muscles contract properly. The sarcomeres are composed of thick and thin muscle filaments, which work in unison by attaching and releasing in a rhythmic manner, allowing the muscles to contract and relax, respectively. This process is necessary for the heart to pump blood
- The following are some known gene functions:
- MYH7: It codes for cardiac β myosin heavy chain, a crucial component of thick filament
- MYBPC3: It codes for cardiac myosin binding protein, associates with the thick filament and provides structural integrity required for contractions
- TNNT2: It codes for cardiac troponin T, which is 1 of the 3 proteins of the troponin complex in thin filaments, required for muscle contractions and relaxations
- TNNI3: It codes for cardiac troponin 1, also a part of the troponin complex
- When there is a mutation in one or many genes involved in this process, it may result in altered proteins or loss of proteins in the sarcomeres, interfering with cardiac function. However, the link between compromised sarcomere function and thickening of cardiac muscles is not well understood
- The mutations are inherited in an autosomal dominant manner
Arrhythmogenic right ventricular Cardiomyopathy (ARVC) is caused by mutations in at least 5 genes involved in the formation and function of desmosomes.
- The 5 genes whose mutation(s) cause ARVC include:
- DSP
- JUP
- PKP2
- DSG2
- And, DSC2
- These genes code for desmoplakin, plakoglobin, plakophilin 2, desmoglein 2, and desmocollin 2 respectively
- Of the 5 genes, PKP2 gene mutations are the most common
Desmosomes establish cell-cell connections in cardiac muscle and epithelial cells. They are highly adhesive and are resistant to mechanical pressure. Under normal circumstances, the desmosomal proteins ensure proper functioning of desmosomes.
- When mutated, the structure of desmosomes disintegrates, particularly with physical exertion
- The muscle cells of the heart separate and disintegrate, paving the way for scar tissue to form, composed mainly of fibrous and fat cells
- The build-up of scar tissue leads to the walls of the right ventricle to stretch uncharacteristically, leading to:
- Inefficient pumping of blood
- Abnormal electrical conductivity in the heart
- ARVC is inherited in an autosomal dominant fashion. However, if associated with mutations causing cardio-cutaneous syndromes, such as Naxos disease and Carvajal syndrome, the condition is inherited in an autosomal recessive manner
Restrictive Cardiomyopathy is caused by mutation(s) in the TNNI3 gene, among several other uncharacterized gene mutations.
- Under normal circumstances, the gene codes for cardiac troponin I protein, which forms the “troponin protein complex” with two other proteins. This complex aids in the contraction and relaxation of the heart muscles in a rhythmic manner
- The mutations in the TNNI3 gene results in the formation of a defective protein that compromises the formation and functioning of the troponin protein complex. This in turn affects the contraction and relaxation of the heart muscles
- The mutation is inherited in an autosomal dominant manner
Dilated Cardiomyopathy can be caused by mutation(s) in over 30 genes, including the TTN gene.
- The TTN gene codes for the protein “titin”, which is involved in the structural integrity and flexibility of sarcomeres, as well as their assembly. A sarcomere is the basic functional unit of heart muscle
- When the gene is mutated, there is an abnormal shorter version of the titin protein synthesized, which is dysfunctional. The exact mechanism of how this causes dilated Cardiomyopathy is unclear
- The majority of mutation gene mutations associated with this subtype are inherited in an autosomal dominant manner. Although, in a few cases, gene mutations are inherited in an autosomal recessive or X-linked manner
Autosomal dominant inheritance pattern: In this type of inheritance, a single copy of a defective gene in every cell of an individual is sufficient to cause the condition. Typically, one inherits the condition from an affected parent.
Autosomal recessive inheritance pattern: In this type of inheritance, an individual must possess both copies of the causative gene in the defective form in every cell of his/her body for the condition to manifest itself. An affected individual inherits one defective copy from each parent. The parents are carriers of the condition and are generally not affected.
X-linked inheritance pattern: In this type of inheritance, the defective gene is carried on the X chromosome. Females have two X chromosomes, and the unaffected gene copy masks the effects of a defective gene copy. However, since males have only one X chromosome inherited from their mother, the defective gene is expressed in them, causing the condition.
Apart from heritable genetic changes, the following can also lead to various subtypes of Cardiomyopathy:
Coronary artery disease: It is the most common cause of dilated Cardiomyopathy.
- It leads to reduced blood supply to the heart muscles
- Injury and necrosis of heart muscles may occur, leading to formation of scar tissue
- The healthy tissue enlarges and extends to keep the muscles working
- The demands of the body are met temporarily. However, the expansion of muscles to balance the function of dead tissue leads to loss of flexibility in the heart muscle
- The heart muscle weakens, causing the condition
Other contributory factors may include:
- Spontaneous mutations, although the exact reason for, and the nature of these mutations is not deciphered
- Chronic high blood pressure, which leads to thickening of the left ventricle
- Previous heart attack, damage to heart tissue
- Prolonged and sustained tachycardia (overworked heart muscles)
- Viral, bacterial, fungal or parasitic infections of the heart muscle can lead to weakening of the heart muscle. In order to keep the heart functioning, the weakened muscle gets over-worked, causing further weakening of the cardiac muscles
- Poorly-controlled diabetes: The exact cause is not known, but diabetes can cause structural changes in the heart
- Thyroid disease: The exact cause of heart muscle thickening as a consequence of decreased or increased thyroid hormone is not understood. Both conditions can cause changes in the consumption of oxygen by heart muscles, as well as muscle contractility in the heart
- Lipodystrophy: It is a genetic condition that results in abnormal formation, storage and distribution of fat. Individuals with a mutation in seipin, an integral membrane protein, exhibits a strong correlation with Cardiomyopathy. The majority of affected individuals have insulin-resistant diabetes, high cholesterol and triglyceride levels, all of which can lead to thickening of the heart muscle
- Acromegaly: Abnormal increase in growth hormone, as a result of a benign pituitary tumor, can cause aberrant growth of external and internal tissue. The thickening of heart muscles is a known outcome of this disorder
- Pheochromocytoma: It is an adrenal gland tumor that can cause acute or chronic high blood pressure in the affected individual. The blood pressure changes are caused by the release of catecholamines, which control involuntary muscle movement in the body, such as those of the heart
- Neurofibromatosis: The tumors formed in this genetic condition are known as neurofibromas that cause high blood pressure to develop in the affected individuals
- Neuromuscular diseases such as muscular dystrophy: Some gene mutations that cause dysfunction of skeletal muscle also cause aberrations in cardiac muscle. Therefore, progressive cardiac malfunctions are often observed with neuromuscular disorders
- Connective tissue disorders, such as rheumatoid arthritis and systemic lupus erythematosus, can cause weakness in heart muscle
- Amyloidosis: It is a systemic disease that results in the build-up of amyloid proteins in tissues and organs, including the heart. This condition is more common in adults
- Endocardial fibroelastosis: It is a disease characterized by an increased thickening in the muscles that layer the heart chambers. This leads to an increase in fibrous tissue in the heart, with a subsequent enlargement of the organ. Endocardial fibroelastosis typically affects infants
- Hemochromatosis: A genetic condition that causes excess iron in the body. This can lead to iron toxicity in many organs, including the heart
- Sarcoidosis, which is a systemic disease that can affect several parts of the body, leading to the growth of small lumps of inflammatory cells. The disease affects the heart by causing abnormal rhythms and electrical conductivity abnormalities
- Hypereosinophilic syndrome (HES): It is a rare type of blood disorder. In this disorder, there is abnormally elevated number of eosinophils, which are a type of white blood cells involved in immune functions. These cells penetrate tissues and organs, including the heart muscles
- Scleroderma, an autoimmune disorder in which an individual’s immune cells destroy his/her own healthy cells
- Tumors in the heart, including those from carcinoid syndrome, which is a rare slow-growing type of tumor predominantly affecting organs of the GI tract
- Chemotherapeutic treatment for cancer, which can generate scar tissue
- Radiation therapy for cancer that can cause scarring of tissues
- Infection by HIV or AIDS is considered to significantly contribute to the development of dilated Cardiomyopathy in the affected individuals
- Alcoholism: Alcohol directly affects the heart muscle. When this is combined with improper nutrition, the effect is deleterious to the heart, causing erratic functioning
- Congenital genetic abnormalities and structural defects in the heart
- Peripartum Cardiomyopathy: It is a heart condition that develops in a woman either late in her pregnancy or within 5 months following delivery of the child. The exact cause of how this condition develops is not clear
- Heavy metal poisoning, due to exposure to metals such as lead, cobalt, arsenic and mercury
- Drug abuse
- Extreme stress that may be physical or emotional
- This can lead to a surge in stress hormone levels, such as those of adrenaline and cortisol
- There is a resultant, rapid increase in heart rate and blood pressure
- This shocks the heart, leading to changes in the heart muscle and/or blood circulation. These changes interfere with the proper contraction of the left ventricle, causing the symptoms
- In women, estrogen plays a protective role in protecting the heart. This is probably the reason the condition is more prevalent in post-menopausal women
What are the Signs and Symptoms of Cardiomyopathy?
The signs and symptoms of Cardiomyopathy may vary among individuals, depending on the subtype of the condition they are affected by. In some cases, the affected individual may be asymptomatic, and a fainting episode may be the first indication of the heart condition.
The commonly noted signs and symptoms of Cardiomyopathy include:
- Chest pain
- Dizziness, fainting (also after physical exertion)
- Shortness of breath, particularly with physical exertion (exertional dyspnea)
- Shortness of breath, while lying down (orthopnea)
- Shortness of breath and coughing while sleeping (nocturnal paroxysmal dyspnea)
- Fatigue
- Palpitations; a sensation of rapid fluttering or pounding heartbeat
- Heart murmurs: It is an unusual sound heard during the heartbeat. This can be an extra beat or whooshing/swishing sound, and may be faint or loud
- Swelling of ankles, legs, abdomen, or veins in the neck
- Low urine output
- Urge to urinate frequently at night (particularly in adults)
- Lack of concentration
- Reduced appetite
How is Cardiomyopathy Diagnosed?
For an accurate diagnosis of Cardiomyopathy, the following tests and exams may be required:
- A thorough physical examination and an assessment of symptoms
- Evaluation of personal and family medical history
- Blood test to check for markers of cardiac disease
- Chest X-ray to check for heart size, contour, and fluid build-up in lungs
- Electrocardiogram (EKG) to check the heart’s electrical activity
- Echocardiography (ECG or echo) uses sound waves to create a moving picture of the heart. This helps to check the size, shape, and pumping function of the heart
- Stress test: This test places stress on the heart by making it work harder and beat faster to determine, if the cardiac muscles can cope with the increased workload
- Cardiac catheterization: To check for pressure and blood flow in the heart’s chambers. It is often coupled with coronary angiography, in which a harmless dye is injected into the coronary arties and with the help of an X-ray, blood flow through heart and blood vessels can be observed
- Myocardial biopsy: A piece of the heart is removed and the cells are investigated for changes that may suggest hypertrophic Cardiomyopathy
- Genetic testing to seek confirmation of the diagnosis, in cases of inherited Cardiomyopathy. This may be recommended for the whole family, which can help understand if the condition is inherited
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Cardiomyopathy?
The following are some potential complications of Cardiomyopathy:
- Heart valve regurgitation: It causes the heart to pump ineffectively, such that blood flows back into the heart
- Arrhythmias: Abnormal heart rhythm, which can be triggered by physical exertion
- Heart failure owing to cardiogenic shock or reduced pumping of blood
- Heart failure that is caused by poor blood flow to the heart
- Ventricular free wall rupture, which is a tear in the muscle wall of the ventricles, and may be fatal
- Sudden cardiac arrest that can be unexpected
- Embolism: Development of blood clots in the heart which may get into the bloodstream and obstruct blood supply to many important organs
- Edema: Fluid buildup in the lungs, abdomen, legs, and feet; all consequences of ineffective heart pumping
- Stroke
- End-stage heart failure, where the heart does not respond to any treatment
How is Cardiomyopathy Treated?
Treatment options depend on the type of Cardiomyopathy and severity of symptoms. The following are some treatment modalities for the disease:
- Bringing about certain lifestyle changes:
- Adhering to a healthy diet that includes fresh fruits, vegetables, whole grains, fish and dairy products
- Engaging in routine physical activity
- Smoking cessation
- Losing excess weight
- Avoiding alcohol and illicit drugs
- Getting enough sleep
- Avoiding or reducing of stress
- Seeking treatment for underlying conditions (such as diabetes, high blood pressure, etc.)
- Beta blockers and calcium channel blockers, generally the first choice of medicines to treat Cardiomyopathies, to regulate heartbeats
- Prescription medications:
- For blood pressure regulation - angiotensin converting enzyme inhibitors and angiotensin II receptor blockers
- Anti-arrhythmogenic drugs to maintain normal heartbeat rhythm
- Medicines to balance electrolytes in the body: Electrolytes are minerals that help the proper functioning of muscles and nerve tissues
- Diuretics to remove excess fluid and sodium
- Anti-coagulants or blood thinners, which prevent blood clot formation
- Anti-inflammatory medications
Non-surgical procedures:
- Alcohol septal ablation:
- Ethanol (a type of alcohol) is injected into a small artery
- The alcohol kills cells in the tissue, to shrink the heart muscle to a more ‘normal’ size
- This improves blood flow through the ventricles, which in turn improves the symptoms
- Pain management with radiofrequency ablation (RFA), which uses a radio wave to produce an electrical current. This current is directed toward a nerve tissue, whose temperature rises and dulls the pain
Surgical procedures:
- Septal myectomy:
- It is a type of open-heart surgery that is typically used for obstructive hypertrophic Cardiomyopathy with severe symptoms
- The procedure is usually recommended for young patients with poor response to medicines
- It helps in improving blood pumping by removing part of the thickened heart muscle
- Surgically-implanted devices such as implantable cardioverter defibrillator (ICD):
- It is a small device implanted in the chest or abdomen and connected to the heart via wires
- The device helps control life-threatening arrhythmias that can lead to sudden cardiac arrest
- Heart transplantation for end-stage heart failure
How can Cardiomyopathy be Prevented?
Currently, it may not be possible to prevent Cardiomyopathy.
- If Cardiomyopathy is caused by an inherited gene mutation, there are no guidelines or specific methods available for preventing it
- Genetic testing of the expecting parents (and related family members) and prenatal diagnosis (molecular testing of the fetus during pregnancy) may help in understanding the risks better during pregnancy
- If there is a family history of the condition, then genetic counseling will help assess risks, before planning for a child
- Active research is currently being performed to explore the possibilities for treatment and prevention of inherited and acquired genetic disorders such as some forms of Cardiomyopathy
- Some lifestyle changes, such as following a healthy diet, quitting cigarettes, reducing alcohol drinking, getting regular exercise, and reducing stress, may help prevent the severity and complications from the disease
- If the disorder is secondary to a pre-existing medical condition, seeking treatment for that condition may help an affected individual reduce the possibility of Cardiomyopathy
- In high-risk individuals, an implantable cardioverter defibrillator may help prevent sudden cardiac arrest, which is a potential complication of Cardiomyopathy
Regular medical screening at periodic intervals with tests and physical examinations are strongly recommended.
What is the Prognosis of Cardiomyopathy? (Outcomes/Resolutions)
The prognosis of Cardiomyopathy is determined by the severity of the condition, overall health of the affected individual, and his/her response to treatment. Without treatment, symptoms can worsen and complications can follow. Therefore, a timely diagnosis and prompt treatment is essential.
- In some cases, sudden cardiac arrest even at first presentation of the condition, may be fatal
- Treatment can prevent worsening of Cardiomyopathy, reduce complications, and control symptoms, with good outcomes
- Also, in some cases, the prognosis may be determined by the seriousness of pre-existing conditions
- The outcome of restrictive cardiomyopathy is poor, since the average survival period after diagnosis is approximately 7 years
- Dilated Cardiomyopathy is a progressive condition; the 5-year survival rates of those affected is reported to be around 30%
- Takutsubo Cardiomyopathy is a transient condition, with most affected individuals recovering within a few weeks
Additional and Relevant Useful Information for Cardiomyopathy:
Please visit our Heart & Vascular Health Center for more physician-approved health information:
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.