What are the other Names for this Condition? (Also known as/Synonyms)
- AML of Skin
- Cutaneous AML
- Cutaneous Angiomyolipoma
What is Angiomyolipoma of Skin? (Definition/Background Information)
- An angiomyolipoma (AML) is a benign tumor that is a mixture of blood vessels (angio-), smooth muscles (myo-), and fat (or lipoma). The tumor is seen among a wide age range of adults and can occur at various locations in the body. But, the most common location is the kidney (renal AML)
- Angiomyolipoma of Skin (or Cutaneous Angiomyolipoma) is a very uncommon extrarenal (not located in the kidney, the usual site) AML that may be present as a subcutaneous swollen lesion in the body. The tumor is seen among a wide age range of individuals, including children and adults
- Angiomyolipoma can be associated with a syndrome (tuberous sclerosis) in some cases, termed syndromic angiomyolipoma; or in a majority of cases, it may not be associated with a genetic disorder, when it is termed non-syndromic angiomyolipoma
- However, all the reported cases of Cutaneous Angiomyolipoma have not occurred against a background of tuberous sclerosis. Currently, only sporadic cases of Cutaneous AML have been reported
- Angiomyolipoma of Skin is usually present in the peripheral locations of the body (fingers and toes) or on the ear. Small tumors are mostly asymptomatic, while large tumors may present pain, discomfort, and even cosmetic issues
- Typically, a surgical excision and removal of Angiomyolipoma of Skin may be undertaken. The prognosis of Cutaneous Angiomyolipoma is generally excellent with suitable treatment, since it is a benign tumor
Who gets Angiomyolipoma of Skin? (Age and Sex Distribution)
- The sporadic (non-syndromic) cases of Angiomyolipoma of Skin have been observed in the age group 33-77 years (average age 53 years)
- Generally, when AML is associated with tuberous sclerosis complex (syndromic cases), the age group in which the tumor is often manifested is between 25-35 years
- In rare cases, AML is observed in children too (mostly of the syndromic type)
- Generally, sporadic angiomyolipomas have a predilection for females; but to the contrary, Cutaneous Angiomyolipomas show a high preference for males (some studies indicate a 7:1 male-female ratio)
- No ethnic or racial preference is seen
What are the Risk Factors for Angiomyolipoma of Skin? (Predisposing Factors)
Currently, no risk factors have been noted for the sporadic cases of Angiomyolipomas of Skin and no cases associated with tuberous sclerosis have been recorded.
Nevertheless, the risk factors for angiomyolipoma may include the following:
- Tuberous sclerosis (TS) is a risk factor for angiomyolipoma, and hence, a family history of TS can increase the risk. Tuberous sclerosis complex is an inherited genetic disorder that can cause the formation of other tumor types, such as astrocytomas, rhabdomyomas, phakomas, oncocytomas, and angiofibromas, at various body locations
- In general, AML can also be associated with other syndromes/disorders including:
- von Recklinghausen disease (neurofibromatosis type I)
- von Hippel-Lindau disease
- Sturge-Weber syndrome
- Autosomal dominant polycystic kidney disease
- Some reports indicate that events causing an hormonal imbalance in the body, such as puberty and pregnancy in women, may be a risk factor
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases one’s chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
What are the Causes of Angiomyolipoma of Skin? (Etiology)
The exact cause and mechanism of Angiomyolipoma of Skin formation, in a majority of cases, is unknown. Solitary tumors are believed to be the result of sporadic mutations on TSC1 or TSC2 genes, implying that they do not have a preceding family history of the condition.
- Research has shown that the tumors arise from cells called perivascular epithelioid cells (PEC), which surrounds the blood vessels. Hence, angiomyolipoma (AML) is a type of a tumor known as a PEComa
- Multiple angiomyolipomas are known to occur in a background of tuberous sclerosis (TS), which is a genetic condition. It may also occur when there is a positive family history of the condition. In the case of Angiomyolipoma of Skin, no such association with TS has been clearly noted
- In general, syndromic AML is also associated with other genetic disorders such as von Recklinghausen disease, von Hippel-Lindau disease, Sturge-Weber syndrome, and autosomal dominant polycystic kidney disease
- Some research indicates that hormonal influence may play a role in AML formation for the following reasons:
- The tumor is more often seen in women
- It grows larger during pregnancy
- The onset can be after puberty
- High progesterone receptor activity is present on microscopic examination
What are the Signs and Symptoms of Angiomyolipoma of Skin?
The signs and symptoms of Angiomyolipoma of Skin vary from one individual to another and may include the following:
- Most tumors are small-sized subcutaneous nodules and may not exhibit any signs and symptoms
- They are also solitary, clearly-defined, and non-invasive in nature
- The cutaneous lesions are noticed in the peripheral (acral) regions, such as on the fingers and toes, in most cases
- Many have been reported to occur in the head and neck region (on the external ear), while some tumors have been located in the thigh and abdomen
- Large tumors (size over 4 cm) may cause pain and discomfort; they may also impede the performance of simple daily tasks, depending on their location
- Tumors tend to grow larger in size during pregnancy
How is Angiomyolipoma of Skin Diagnosed?
A diagnosis of Angiomyolipoma may involve the following tests and procedures:
- Complete physical exam with evaluation of medical history
- Radiological imaging studies, such as ultrasound, CT, MRI scans, of the affected region
- Vascular angiographic studies of the tumor
- Dermoscopy: It is a diagnostic tool where a dermatologist examines the skin using a special magnified lens
- Wood’s lamp examination: In this procedure, the healthcare provider examines the skin using ultraviolet light. It is performed to examine the change in skin pigmentation
- Additional tests may be necessary to rule out any underlying condition, if any
Although the above modalities can be used to make an initial diagnosis, a tissue biopsy of the tumor is necessary to make a definitive diagnosis to begin treatment. The tissue for diagnosis can be procured in multiple different ways which include:
- Fine needle aspiration (FNA) biopsy of the tumor: A FNA biopsy may not be helpful, because one may not be able to visualize the different morphological areas of the tumor. Hence, a FNA biopsy as a diagnostic tool has certain limitations, and an open surgical biopsy is preferred
- Core biopsy of the tumor
- Open biopsy of the tumor
Skin biopsy:
- A tissue biopsy of the tumor is performed and sent to a laboratory for a pathological examination. A pathologist examines the biopsy under a microscope. After putting together clinical findings, special studies on tissues (if needed) and with microscope findings, the pathologist arrives at a definitive diagnosis. Examination of the biopsy under a microscope by a pathologist is considered to be gold standard in arriving at a conclusive diagnosis
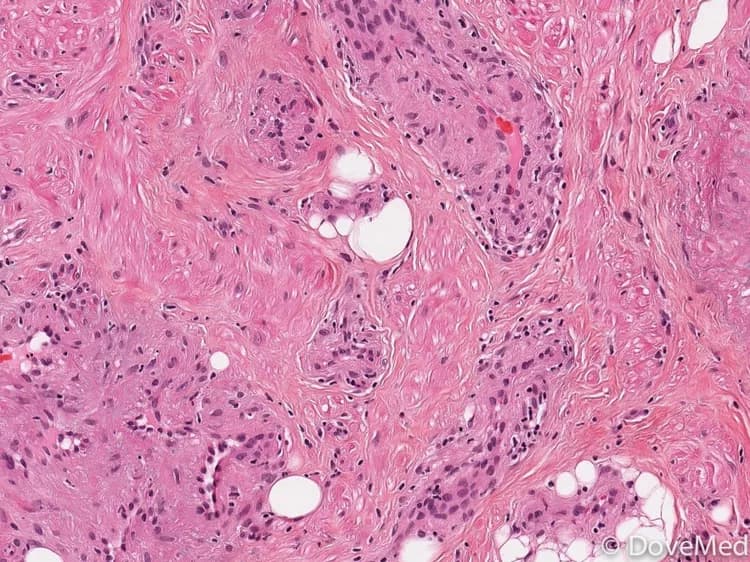
- Biopsy specimens are studied initially using Hematoxylin and Eosin staining. The pathologist then decides on additional studies depending on the clinical situation
- The tumors may have varying proportions of blood vessels, smooth muscle, and fat cells, when examined by a pathologist under a microscope
- Sometimes, the pathologist may perform special studies, which may include immunohistochemical stains, molecular testing, and very rarely, electron microscopic studies to assist in the diagnosis
Note: A differential diagnosis, to eliminate other tumor types is considered, before arriving at a conclusion.
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
What are the possible Complications of Angiomyolipoma of Skin?
The complications are dependent on the site and size of the tumor. The complications of Angiomyolipoma of Skin may include:
- Cosmetic issues and stress, especially due to tumors on the face or hands
- Large tumor masses may get secondarily infected with bacteria or fungus
- Damage to the muscles, vital nerves, and blood vessels, during surgery
- Post-surgical infection at the wound site is a potential complication
- Research has not conclusively proven that angiomyolipoma can turn malignant. Although, some cases of sarcoma developing from AML (not associated with tuberous sclerosis) have been noted
How is Angiomyolipoma of Skin Treated?
The treatment measures for Angiomyolipoma of Skin may include the following:
- Majority of asymptomatic tumors are not surgically removed: The healthcare provider may recommend a ‘wait and watch’ approach for small-sized tumors presenting mild signs and symptoms, after a diagnosis of angiomyolipoma is established
- Surgical intervention with complete excision can result in a complete cure. It can also help reduce the chances of tumor recurrence
- Tumor embolization (performed on a case-by-case basis) is a possible treatment option. Here the blood supply to the tumor is blocked resulting in its shrinkage or death
- Everolimus is FDA approved for use in TSC-associated renal Angiomyolipomas. It does not have FDA approval for use in AML of Skin
- Post-operative care is important: A minimum activity level is to be ensured, until the surgical wound heals
Follow-up care with regular screening may be recommended by the healthcare provider.
How can Angiomyolipoma of Skin be Prevented?
Current medical research has not established a method of preventing Angiomyolipoma of Skin. However, in case it is associated with genetic disorders, such as tuberous sclerosis, then the following may be considered:
- Genetic testing of the expecting parents (and related family members) and prenatal diagnosis (molecular testing of the fetus during pregnancy) may help in understanding the risks better during pregnancy
- If there is a family history of the condition, then genetic counseling will help assess risks before planning for a child
- Active research is currently being performed to explore the possibilities for treatment and prevention of inherited and acquired genetic disorders such as tuberous sclerosis
- Regular medical screening at periodic intervals with tests and physical examinations are strongly recommended
What is the Prognosis of Angiomyolipoma of Skin? (Outcomes/Resolutions)
The prognosis of Angiomyolipoma of Skin depends upon the severity of the signs and symptoms. In most cases, the prognosis of small-sized solitary tumors is excellent with surgical intervention or appropriate treatment, since these are benign tumors.
Additional and Relevant Useful Information for Angiomyolipoma of Skin:
Angiomyolipoma can occur at various locations in the body, such as the soft tissue, uterus, fallopian tube, spermatic cord, penis, liver, and lung.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals


0 Comments
Please log in to post a comment.