Study Compares Cognitive Outcomes For Treatments Of Brain Lesions
Among patients with 1 to 3 brain metastases, the use of stereotactic radiosurgery (SRS) alone, compared with SRS combined with whole brain radiotherapy, resulted in less cognitive deterioration at 3 months, according to a study appearing in the July 26 issue of JAMA.
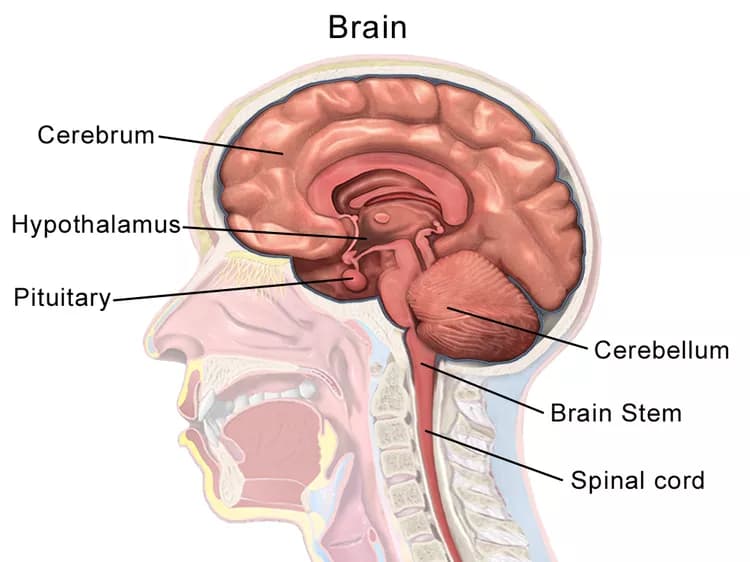
Approximately 30 percent of patients with cancer develop brain metastases, and the incidence of these lesions is rising. Most patients present with limited intracranial metastases, usually defined as 1 to 3 lesions. Stereotactic radiosurgery is an effective and commonly used treatment for brain metastases, but intracranial tumor progression is frequent after SRS alone, primarily because of the development of new metastatic lesions. Whole brain radiotherapy (WBRT) significantly improves tumor control in the brain after SRS, yet because of its association with cognitive decline, its role in the treatment of patients with brain metastases remains controversial.
Paul D. Brown, M.D., of Mayo Clinic, Rochester, Minn., and colleagues conducted a study in which 213 patients with 1 to 3 brain metastases were randomly assigned to receive SRS alone (n = 111) or SRS plus WBRT (n = 102). The study was conducted at 34 institutions in North America; average patient age was 61 years. The primary outcome measured for the study was cognitive deterioration among patients who completed assessments at study entry and 3 months. Other measured outcomes included quality of life, functional independence, long-term cognitive status, and overall survival.
The researchers found that there was less cognitive deterioration at 3 months after SRS alone (40/63 patients [64 percent]) than when combined with WBRT (44/48 patients [92 percent]. Quality of life was higher at 3 months with SRS alone, including overall quality of life. There was no significant difference in functional independence at 3 months between the treatment groups. Median overall survival was 10.4 months for SRS alone and 7.4 months for SRS plus WBRT. For long-term survivors, the incidence of cognitive deterioration was less after SRS alone at 3 months and at 12 months.
"In the absence of a difference in overall survival, these findings suggest that for patients with 1 to 3 brain metastases amenable to radiosurgery, SRS alone may be a preferred strategy," the authors write.
Editorial: Whole Brain Radiotherapy for Brain Metastases
"The debate between WBRT and SRS has been resolved for the specific type of patient (with 1-3 metastases) who enrolled in the current study, and there is little role for WBRT for these patients," write Carey K. Anders, M.D., of the University of North Carolina at Chapel Hill, and colleagues in an accompanying editorial.
"However, both treatment modes have a valid position in clinical practice because many patients do not precisely fit the characteristics for study entry. Thus, based on the robust findings from the current study and until proven otherwise, WBRT may still have an important role for treatment of patients who are not in this specific disease category (i.e., 1-3 brain metastases). However, the study results cannot be extrapolated to infer that SRS is the standard for patients with 4 or more metastases or that WBRT no longer has a role in the treatment of brain metastases."
The above post is reprinted from materials provided by The JAMA Network Journals. Note: Content may be edited for style and length.
Disclaimer: DoveMed is not responsible for the adapted accuracy of news releases posted to DoveMed by contributing universities and institutions.
Primary Resource:
- Brown, P. D., Jaeckle, K., Ballman, K. V., Farace, E., Cerhan, J. H., Anderson, S. K., ... & Ménard, C. (2016). Effect of Radiosurgery Alone vs Radiosurgery With Whole Brain Radiation Therapy on Cognitive Function in Patients With 1 to 3 Brain Metastases: A Randomized Clinical Trial. JAMA,316(4), 401-409.
- McTyre, E., Scott, J., & Chinnaiyan, P. (2013). Whole brain radiotherapy for brain metastasis. Surgical neurology international, 4(Suppl 4), S236.
Related Articles
Test Your Knowledge
Asked by users
Related Centers
Related Specialties
Related Physicians
Related Procedures
Related Resources
Join DoveHubs
and connect with fellow professionals

0 Comments
Please log in to post a comment.